Introduction
This blog is based on the Pain Education Theory & Practice course on Embodia Academy with Debbie Patterson, PT, Geoff Bostick, PT, PhD, and the Pain Science Division of the CPA, as well the the Pain Education Theory and Practice - Introductory Course.
With the growing research and support for pain education, it is becoming one of the most essential components of a patient’s treatment plan.
Registered physiotherapists Debbie Patterson and Geoff Bostick provide several online physiotherapy courses that address the important gaps in knowledge surrounding the theory and practice of pain education.

Maladaptive beliefs and thoughts about pain are substantial barriers to recovery.

Pain education can help address these thoughts by providing current and relevant science specifically targeted to the individual patient's needs and level of understanding.
Appropriate education can be a core intervention for changing pain and quality of life.
What is Pain Education?
Pain education is a type of intervention to help people cope with their pain by understanding how pain is processed neurophysiologically.

When providing pain education, we must adopt a biopsychosocial approach when educating our patients about pain science, as research suggests there are long-term clinical improvements in pain when doing so.
Furthermore, by applying a biopsychosocial approach, there are a variety of different factors that we can address to help cope with their pain, besides the damaged tissue or perceived damaged tissue.
There are Two Main Parts of Pain Education:
Short interventions and discrete interventions.
Short intervention refers to strategies that permeate through all treatment sessions and are often provided to all patients, such as reassurance.
Discrete interventions are more specific in helping people understand how pain is processed neurophysiologically by providing a different point of view on how pain works and challenging some traditional views on pain.
Here Are Some Key Things You Can Do as a Practitioner:
- Reflect on our perspectives and beliefs on pain. Often, therapists' fear-avoidance beliefs may rub off on patients.
- The patient is the expert; physiotherapists assist them. Patients bring a lot of expertise about their pain, and we need to acknowledge it and give them space to discuss it
- Take a biopsychosocial approach. Although many students and clinicians know theoretically what the biopsychosocial approach is, when it comes to doing it, we revert to the biomedical model. This may lead to problems, as some of the messages for pain education contradict the biomedical model.
- Pain is normal, personal, and always real. Your patients, and almost everyone, need to hear this.
- Pain and tissue damage rarely relate. Pain is a response from your nervous system to what it judges to be threatening. Evidence suggests persistent pain is a wiring problem, and not a tissue damage problem
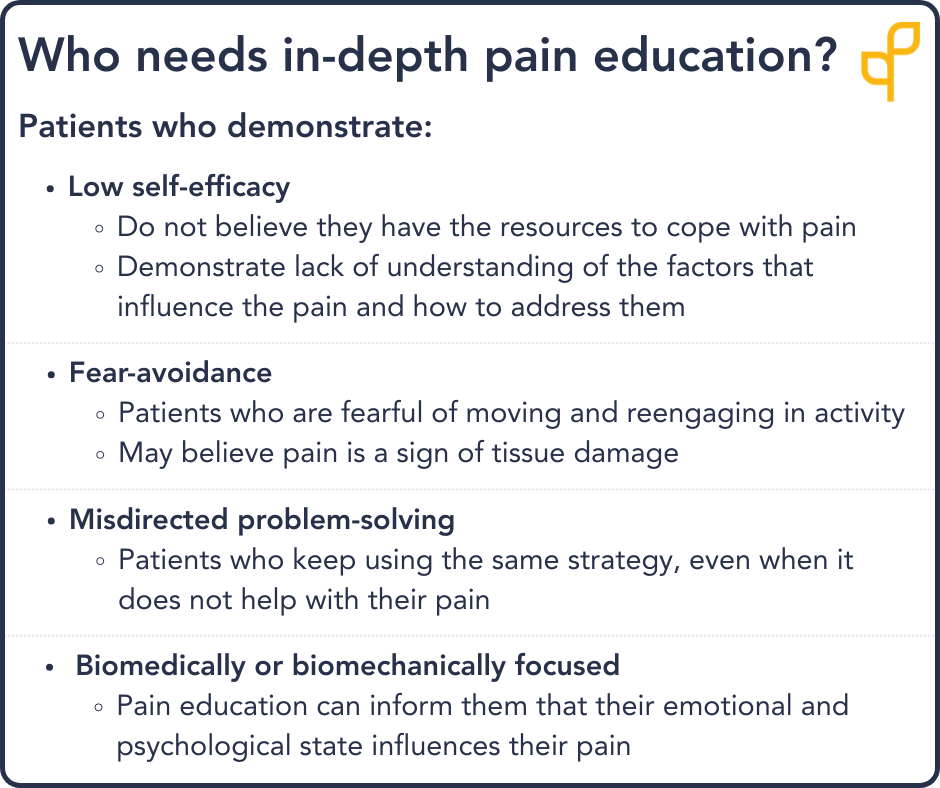
Does Everyone Need Pain Education?
Yes and no.
Remember that pain education has both short and discrete interventions.
Most patients will benefit from short interventions, whereas not everyone may need a discrete pain education intervention.
Conducting a thorough subjective and objective assessment will be your best strategy in determining if your patient needs a discrete pain education intervention.
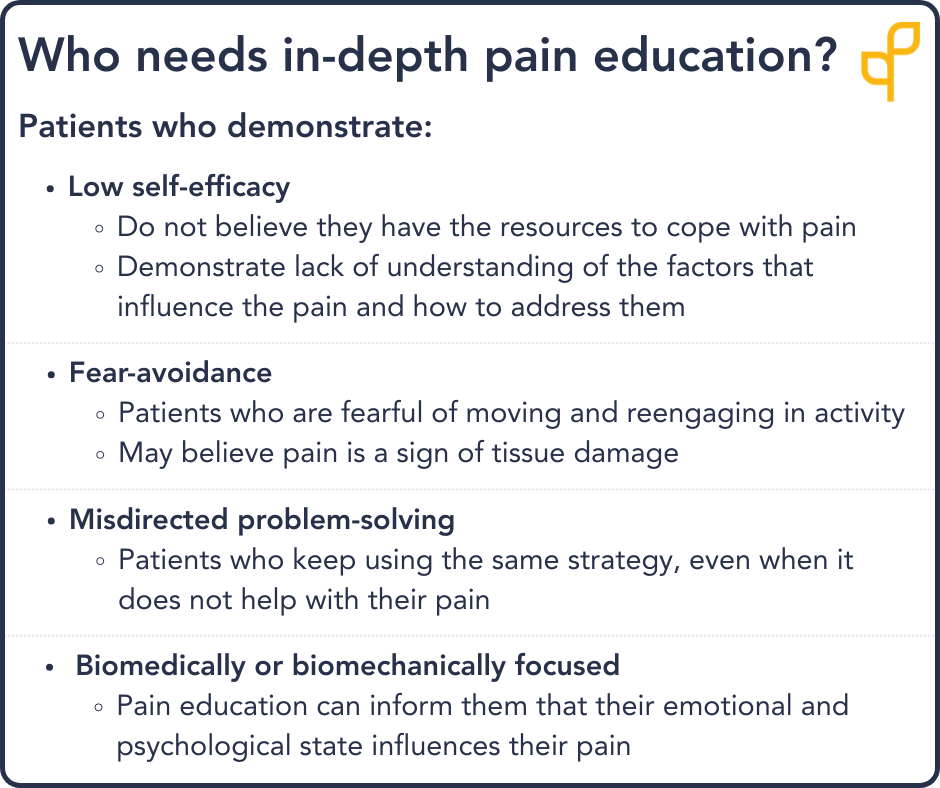
Patients who may not require in-depth pain education include:
- Patients with non-complex pain
- Patients with adaptive thinking, coping, and behaviour
3 Important Components of Pain Education
Here are some important components of pain education:
1. Initial Assessment
- A thorough history, including the opportunity for the patient to disclose their pain
- Red flag screening
- A thorough examination of their neurological status
- A thorough examination of their movement
2. Pain Outcome Measures
It is important to utilize pain outcome measures to be able to track and document any changes throughout the treatment plan.
A few Pain Outcome Measures mentioned in the courses:
McGill Pain Questionnaire
- A self-reported measure of pain that assesses both the quality and intensity of pain
- Can be used to monitor pain over time in a number of diagnoses, including Musculoskeletal Conditions, Chronic Pain, Cancer, Back Pain, Arthritis and Non-Specific Patient Population
Pain Catastrophizing Scale (Available for Embodia Tier 2 & 3 members)
- The self-reported measure used to quantify a patient’s pain experience about their thoughts on pain and how they feel when they are in pain
- Can be completed even when the patient is not in pain
Fear Avoidance Beliefs Questionnaire (Available for Embodia Tier 2 & 3 members)
- A self-reported measure of how a patient’s fear-avoidance beliefs about physical activity and work may impact their pain
-
3. Information Delivery on Pain Looks Different for Everyone
- Some people may want to have a lot of the content knowledge, whereas other people may want it to be more contextualized, specific to them.
- Information can be sprinkled throughout treatment or can be a whole treatment session itself.
To Close
---
Date published: 8 February 2021
Last update: 17 Dec 2025